Dosimetric Comparison of Bolus and Non-Bolus Techniques in Post-Mastectomy Breast Radiotherapy
Authors: Md. Mokhlesur Rahman, Md. Jobairul Islam, Sirajum Munira
Institution: Gono Bishwabidyalay
Introduction
Breast cancer is the leading cause of cancer-related mortality in women globally, with a significant burden in Asia. Post-mastectomy radiotherapy (PMRT) is vital for reducing locoregional recurrence (LR) and improving survival in breast cancer patients. The use of a bolus in PMRT to enhance surface dose is debated due to potential increased skin toxicity. This study aims to compare the dosimetric outcomes of bolus and non-bolus techniques, focusing on skin dose, target coverage, and dose homogeneity.
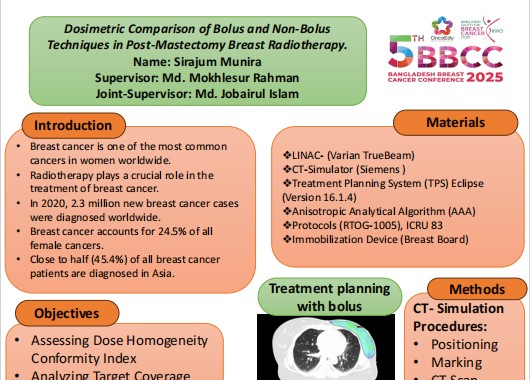
Methods
Five early-stage breast carcinoma patients (stages I-II) underwent PMRT with both bolus and non-bolus techniques. CT Simulation was done using breast board where prescribed dose of 40 Gy in 15 fractions. All treatment plans were created using IMRT and VMAT techniques with the Eclipse Treatment Planning System with Anisotropic Analytical Algorithm (AAA). Dosimetric parameters, including D99%, V95%, Max dose, Mean dose, Conformity Index (CI), and Homogeneity Index (HI), were evaluated for the planning target volume (PTV) and Organ at risk (OAR) doses, including the heart, ipsilateral lung, contralateral lung, and contralateral breast, were analyzed to compare the impact of each technique.
Results
Both bolus and non-bolus techniques provided adequate PTV coverage, with D99% values of 98.17% and 97.14%, respectively, and similar V95% values, indicating no significant compromise in target volume coverage with the non-bolus approach. The non-bolus technique showed slightly better conformity (mean CI: 1.18) compared to the bolus technique (mean CI: 1.25). However, the non-bolus technique favored reduced skin toxicity while achieving adequate dose homogeneity.
Conclusion
While both bolus and non-bolus techniques in PMRT achieved sufficient PTV coverage, the non-bolus approach may offer advantages in terms of reduced skin toxicity without significantly compromising target volume coverage. Bolus may be indicated in cases with high risk of locoregional recurrence in the skin but may not be necessary for all patients.